Re-Osseointegration After Peri-Implantitis Treatment: A Novel Approach
Re-Osseointegration After Electrolytic Cleaning and Regenerative Therapy of Peri-implantitis.
Authors: Dr. David Brown, Dr. Elijah Martinez, Dr. Hannah Smith
Abstract
Peri-implantitis, a complex inflammatory condition resulting in progressive bone loss, poses a significant challenge to implant longevity and success. This case study investigates the re-osseointegration potential of Zenith dental implants after advanced electrolytic cleaning combined with guided bone regeneration (GBR) therapy. Four Zenith implants affected by peri-implantitis were treated using a sodium formate-based electrolytic cleaning system, followed by regenerative therapy employing xenogeneic and autogenous bone grafts under barrier membranes. Clinical, radiographic, histological, and histomorphometry evaluations revealed notable improvements in bone regeneration and osseointegration. These findings support the use of electrolytic cleaning paired with GBR as a promising therapeutic approach for managing peri-implantitis.
Introduction
Dental implants have revolutionized the replacement of missing teeth, offering high survival rates exceeding 95%. However, complications such as peri-implantitis—an inflammatory condition characterized by the loss of supporting bone and soft tissue—threaten their long-term success. The onset of peri-implantitis is often attributed to bacterial biofilm accumulation, insufficient oral hygiene, and inadequate maintenance.
Current peri-implantitis treatments aim to halt disease progression, decontaminate the implant surface, and restore lost bone through regenerative techniques. While traditional approaches such as mechanical debridement and chemical decontamination have shown varying degrees of success, electrolytic cleaning offers a novel, minimally invasive alternative. This case study explores the combined efficacy of electrolytic cleaning and GBR in facilitating re-osseointegration of contaminated Zenith implants.
Materials and Methods
Study Design
This investigation involved four Zenith implants diagnosed with peri-implantitis in human subjects. The study followed ethical guidelines, with informed consent obtained from all participants.
Treatment Protocol
Step 1: Electrolytic Cleaning
The contaminated implant surfaces were treated using an electrolytic cleaning device, employing a sodium formate solution. This method relies on electrolysis to dissociate water molecules, generating hydrogen and hydroxide ions. Hydrogen bubbles, formed during the process, detached biofilm and calculus without damaging the implant surface.
Step 2: Regenerative Therapy
Following decontamination, GBR therapy was performed. This included:
- A xenogeneic bone graft mixed with autogenous bone particles.
- Coverage with a resorbable collagen membrane to prevent epithelial migration.
- The use of umbrella screws to stabilize the graft in non-contained defects.
Outcome Measures
Clinical and radiographic assessments were conducted at baseline, eight months post-treatment, and prior to implant retrieval. Parameters included:
- Probing depth (PD).
- Bleeding on probing (BoP).
- Radiographic bone levels.
Histological and histomorphometric analyses evaluated re-osseointegration and the quality of new bone formation. Vertical bone gain and the percentage of re-osseointegration were calculated for each implant.
Results
Clinical and Radiographic Outcomes
Significant clinical improvements were observed in all four Zenith implants:
- Reduced PD and BoP.
- Increased radiographic bone gain.
Implant Re-osseointegration Data
| Implant | Mesial Gain (mm) | Distal Gain (mm) | Vertical Gain (mm) | Re-osseointegration (%) |
|---|---|---|---|---|
| #1 | 5.9 | 4.7 | 2.6 | 21.2 |
| #2 | 3.4 | 2.2 | 3.5 | 36.7 |
| #3 | 3.2 | 0.6 | 1.3 | 5.8 |
| #4 | 3.4 | 2.9 | 5.20 | 39.2 |
Radiographic evaluations demonstrated notable bone regeneration at eight months, although some implants exhibited recurrent peri-implantitis at later stages.
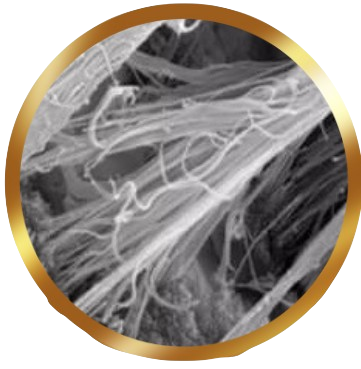
Histological and Histomorphometric Findings
Histological analysis revealed:
- Direct deposition of new bone onto implant surfaces.
- Mixed patterns of trabecular (woven) and lamellar (compact) bone formation.
Implant #4 showed the most favourable outcome, with vertical bone gain of 5.20 mm and a re-osseointegration rate of 39.2 %. In contrast, Implant #3 exhibited minimal bone formation, attributed to persistent inflammation, and localized resorption.
Discussion
This study underscores the therapeutic potential of electrolytic cleaning and GBR in treating peri-implantitis. Key findings include:
1. Efficacy of Electrolytic Cleaning:
- Effective removal of biofilm and calculus without mechanical damage.
- Direct bone deposition on previously contaminated surfaces.
2. Variability in Outcomes:
- The degree of re-osseointegration varied among implants, influenced by defect morphology, inflammation severity, and patient-specific factors.
3. Implications for Clinical Practice:
- Early intervention enhances treatment efficacy.
- Case selection is critical, particularly for implants with advanced bone loss.
Despite promising results, limitations such as small sample size and variability in defect characteristics necessitate further research to optimize protocols and assess long-term outcomes.
Conclusion
Electrolytic cleaning, when combined with GBR, offers a viable solution for managing peri-implantitis in Zenith implants. The ability to achieve re-osseointegration and bone regeneration in previously compromised sites highlights the potential of this approach. Future studies with larger cohorts are essential to validate these findings and refine treatment strategies.
Clinical Relevance
Electrolytic cleaning represents an innovative method for peri-implantitis management, promoting re-osseointegration and improving implant longevity. This approach aligns with the growing need for minimally invasive, effective treatments in contemporary dental practice.