The Importance of Preserving the Peri-Implant Soft Tissue Barrier
Authors: Dr. Moreno Lorso, Dr. David Brown, Dr. Abel K. Miller
Co-authors: Dr. Jacob F. Cooper, Dr. Elijah Martinez, Dr. Hannah Smith
Abstract
This article discusses the critical role of the peri-implant soft tissue barrier in the long-term success of dental implants. The peri-implant mucosal barrier is a biological structure that protects the underlying bone and implant system from bacterial infiltration and mechanical stress. This paper compares the soft tissue dynamics of natural teeth and implants, highlights prosthodontic strategies to mitigate peri-implant disease, and introduces innovations in implant design tailored for soft tissue preservation.
1. Peri-Implant Soft Tissue Interface
The peri-implant soft tissue barrier functions as a protective layer, safeguarding the implant site from external stressors and microbial infiltration. Unlike the periodontal tissue surrounding natural teeth, peri-implant tissues have anatomical and vascular limitations that make them more vulnerable to complications.
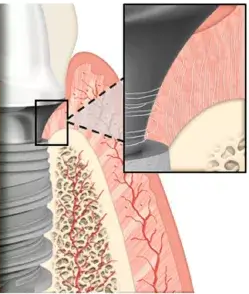
The soft tissue interface comprises:
- Sulcular epithelium: A protective layer that resists bacterial infiltration.
- Junctional epithelium: Forms a tight seal around the implant to minimize microbial invasion.
- Connective tissue attachment: Lacks the perpendicular Sharpey’s fibers found in natural teeth, resulting in weaker mechanical stability.
Blood Supply and Vascularization
In natural teeth, periodontal ligaments provide a rich blood supply, enhancing the tissue’s resilience and regenerative capacity. Conversely, the absence of periodontal ligaments in peri-implant tissues results in reduced vascularization, which can hinder the healing process and compromise defense against pathogens.
Implications for Implant Health
The fragile nature of the peri-implant mucosal barrier underscores the need for meticulous soft tissue management. Disruption to this barrier can accelerate the onset of peri-implant diseases, such as mucositis and peri-implantitis.
2. Prosthodontic Considerations for Soft Tissue Management
Minimizing Tissue Disruption
Traditional bone-level implant procedures often involve repeated abutment disconnections, which can damage the mucosal barrier. Studies have shown that each disconnection disrupts the epithelial seal and connective tissue attachment, leading to inflammation and potential bone resorption.
Clinical Observations
- Epithelial damage: Repeated manipulation exposes underlying connective tissues to bacterial colonization.
- Biological width compromise: Apical migration of the soft tissue attachment increases susceptibility to peri-implant complications.
Innovative implant designs with stable, non-removable abutments can mitigate these risks by preserving the biological width and minimizing soft tissue trauma during prosthetic stages.
3. Clinical Recommendations
Soft Tissue Thickness and Keratinization
Scientific evidence suggests that a minimum soft tissue thickness of 2 mm is critical for implant stability. Thin mucosa or inadequate keratinized gingiva can be addressed with soft tissue grafting procedures to enhance peri-implant health.
Zenith Implant Solutions for Soft Tissue Preservation
Zenith’s implant systems incorporate design features aimed at optimizing soft tissue health:
- Fixed Base Abutments: These eliminate the need for multiple disconnections, preserving the mucosal seal throughout the treatment process.
- Platform Shifting: This minimizes mechanical stress on the crestal bone, reducing the risk of bone resorption.
- Conical Connections: Enhancing stability and ensuring a tight seal against bacterial infiltration.
Zenith’s advanced prosthetic components, including multi-height abutments and tissue-friendly materials, are designed to support natural soft tissue healing and long-term stability.
4. Conclusion
The peri-implant soft tissue barrier is integral to the success and longevity of dental implants. Innovations in implant design, such as Zenith’s fixed base abutments and conical connections, address the unique challenges posed by peri-implant tissue dynamics. By preserving the biological width and minimizing disruption, Zenith Implants provide a comprehensive solution for reducing peri-implant complications and enhancing clinical outcomes.
Clinicians must prioritize soft tissue preservation at every stage of treatment to ensure optimal implant health and patient satisfaction.
.